Bone Health Changes with Age and Menopause
As women approach and go through menopause, a lot changes. Not just hormones, but also how the body maintains its bones. You might hear words like osteopenia and osteoporosis and wonder what they really mean, how serious they are, and what you can do to protect yourself.
The good news? There’s a lot you can do, and it’s never too late to start.
Why Bone Health Changes with Age
Our bones are living tissue. They’re constantly being broken down and rebuilt through a process called remodelling. In our younger years, the rebuilding process easily keeps up with the breakdown, so bone density stays strong.
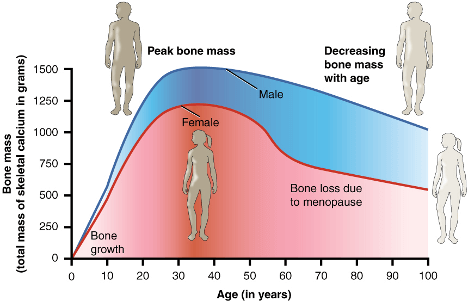
Women typically reach peak bone mass in their late 20s or early 30s. After that, bone density gradually starts to decline. The real turning point happens during and after menopause, when oestrogen levels drop sharply.
🩸 The Role of Oestrogen
Oestrogen helps keep a healthy balance between the cells that break down bone (osteoclasts) and those that build new bone (osteoblasts).
When oestrogen levels fall, bone breakdown speeds up, while bone formation slows down — leading to a rapid loss in bone density.
What Is Osteopenia And How It Leads to Osteoporosis
Osteopenia is when your bone density is lower than normal, but not low enough to be classed as osteoporosis. Think of it as an early warning sign.
Osteoporosis is when bones become fragile and porous, increasing the risk of fractures, even from small bumps or falls.
Many women develop osteopenia around menopause. Without the right interventions, this can progress to osteoporosis over time.
How Menopause Affects Bone Density
Below is a graph of how bone density typically changes across a woman’s lifespan compared to men:
As you can see, bone density stays stable through early adulthood, then declines gradually — but the rate of loss sharply increases around menopause as oestrogen drops.
Research suggests that women can lose up to 2–3% of bone density each year during the first few years after menopause (Frontiers in Public Health, 2022).
What You Can Do to Protect Your Bones
🏋️♀️ 1. Resistance and Strength Training
One of the most powerful tools you have is resistance training - lifting weights or using resistance bands.
Research shows that women who include regular strength training can maintain or even increase bone density, while those who remain inactive continue to lose it.
A study in Osteoporosis International found that postmenopausal women who performed high-intensity resistance and impact training improved their spine bone density by about 4% in just eight months.
In contrast, women who did no resistance training lost nearly 3–4% over the same period.
This is thanks to Wolff’s Law — the principle that bones adapt to the stress placed upon them. In other words, when you safely challenge your bones, they respond by getting stronger.
💡 So when someone says “Don’t lift weights — it’s bad for your joints,” it’s usually the opposite that’s true!
Properly supervised loading strengthens not only your muscles but your bones too.
🥦 2. Nutrition That Supports Bone Health
Exercise is essential — but your body also needs the right nutrients to rebuild stronger bone tissue.
Focus on:
Calcium: Found in dairy, fortified plant milks, leafy greens, and almonds.
Vitamin D: Helps your body absorb calcium. You get it from sunlight and certain foods, or supplements if levels are low.
Protein: Crucial for maintaining muscle, which helps protect your bones.
Magnesium & Vitamin K2: These nutrients support bone metabolism but don’t replace the need for exercise.
🧴 Myth Bust: Supplements alone won’t prevent osteoporosis. They help, but only as part of a bigger picture that includes resistance training, balance, and movement.
🚶♀️ 3. Balance and Posture
As bones weaken, posture often changes, sometimes leading to a forward “hunch” caused by small vertebral fractures (kyphosis).
Exercises that strengthen the back extensors, improve balance, and enhance coordination are key to maintaining posture and independence.
Falls are the most common cause of fractures in older women. Each year, falls lead to thousands of hospital admissions, but strength and balance training dramatically reduce this risk.
💊 4. Other Supports
Hormone Replacement Therapy (HRT): Can help reduce bone loss by restoring oestrogen levels. If appropriate, speak with your GP to see if it’s right for you.
Lifestyle Choices: Avoid smoking, limit alcohol, and keep body weight in a healthy range. Very low weight increases fracture risk.
If You’re Already Noticing Postural Changes
If you’re developing a slight hunchback or rounded shoulders, don’t panic, you can still take action.
An exercise physiologist can help design a safe, evidence-based program focusing on spinal strength, mobility, and posture correction to prevent further collapse..
Takeaway: It’s Never Too Late to Strengthen Your Bones
Menopause doesn’t have to mean frailty. While oestrogen loss does accelerate bone decline, strength training, proper nutrition, balance work, and lifestyle changes can dramatically reduce, or even reverse, the loss.
Remember:
🦴 “A bone that is placed under pressure will reinforce itself.” — Wolff’s Law
So rather than avoiding movement, the goal is to move wisely — load your bones safely, stay consistent, and seek guidance when needed.
References
Endocrine Society. Menopause and Bone Loss. endocrine.org
Frontiers in Public Health (2022). Bone Health and Aging in Women. frontiersin.org
Watson, S. et al. (2017). High-Intensity Resistance and Impact Training Improves Bone Density in Postmenopausal Women. Osteoporosis International.
NIH Osteoporosis and Related Bone Diseases National Resource Center. nih.gov